Medicare Risk Adjustment: Overview & Key Dates for 2023

Medicare Risk Adjustment (MRA) refers to the process of adjusting Medicare patient risk scores according to diagnostic codes assigned to them by healthcare professionals. Risk adjustment is critical so that health plans are adequately funded according to patient needs. The process of risk adjustment also ensures that, regardless of a patient’s demographic information, the funds available to provide care for Medicare beneficiaries with complex medical conditions will flow from the Center for Medicare and Medicaid Service (CMS) to the beneficiary’s health plan and be available to pay providers for medical services.
Understanding Medicare Risk Adjustment
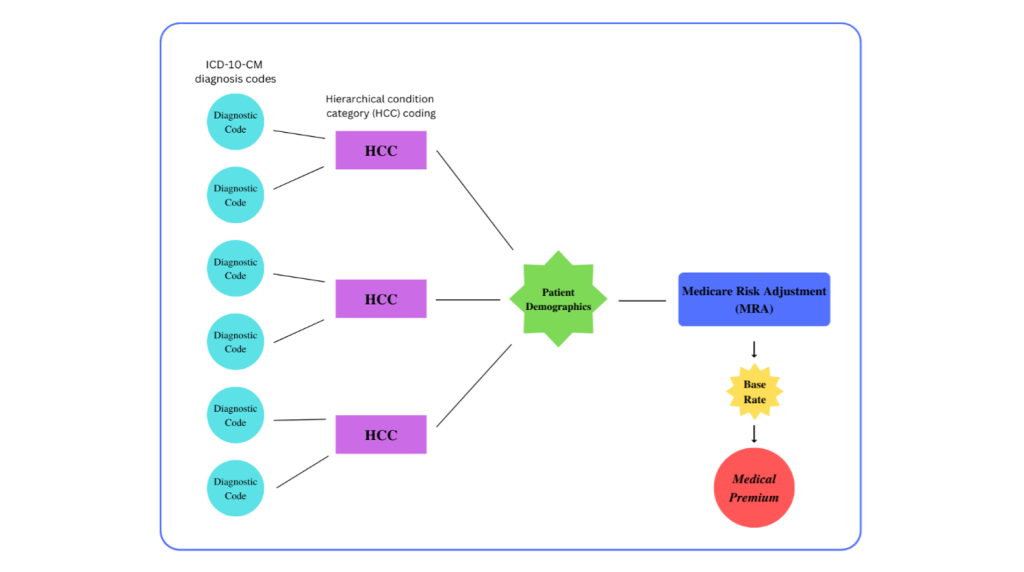
In 2004, CMS implemented Hierarchical Condition Category Coding, better known as HCC Coding, to help estimate and budget for the healthcare costs of Medicare enrollees each coming year.
The implementation process involved building and testing a model based on diagnosis codes clustered into groups to understand variables that predict total cost. While building the model, researchers analyzed thousands of ICD 10 codes and mapped approximately 9,500 to 86 Hierarchical Condition Categories (HCC).
Each of the HCCs have a value attached to them, and when a patient’s various HCC codes are determined, their Medicare Risk Adjustment (MRA) score and demographic information, including age, gender, and additional factors, adjust the base rate into an appropriate medical premium.
Medicare Advantage plans, the Medicare Shared Savings Program, Medicaid, and private health plans use the CMS-HCC risk adjustment model to calculate the health mix of their member enrollment and the reimbursements they can expect from CMS.
Prospective, Concurrent and Retrospective Modeling
As stated in our previous article, CMS started the Risk Adjustment Payment System (RAPS) program to “determine a Medicare Advantage member’s premium on a prospective basis.”
The word “prospective” refers to one of three varieties of HCC review: Prospective, Concurrent and Retrospective.
Prospective-based reviews consist of building a Medicare patient’s profile according to the diagnosis codes they earned during the prior year. Coders evaluate various aspects of the patient’s profile, including hospital records, lab results, demographic information, and physician notes. For example, if a patient was diagnosed with diabetes in 2022, their risk adjusted “score” would rise in 2023, and this would cause their medical premium to increase. Coders and others involved in risk adjustment are predicting the needs of patients via prospective-based review of their assigned HCC codes.
Concurrent reviews happen in real time, as coders review medical notes and HCC codes before the claims are submitted. This work ensures smoother prospective and retrospective modeling because concurrent medical record keeping (with special attention to whether the correct code is used, code trumping, etc.) saves time and energy in the long run.
Retrospective reviews occur annually by CMS after patient care has been delivered and claims have been submitted to the payer. This review typically occurs between October to March. HCC codes may be dropped after this review if the codes do not accurately reflect the patient’s medical records.
Implementing at least one of these HCC coding review processes help health plans receive accurate compensation for the care their organizations provide, though it is often recommended that a combination of reviews take place each year.
Key Dates
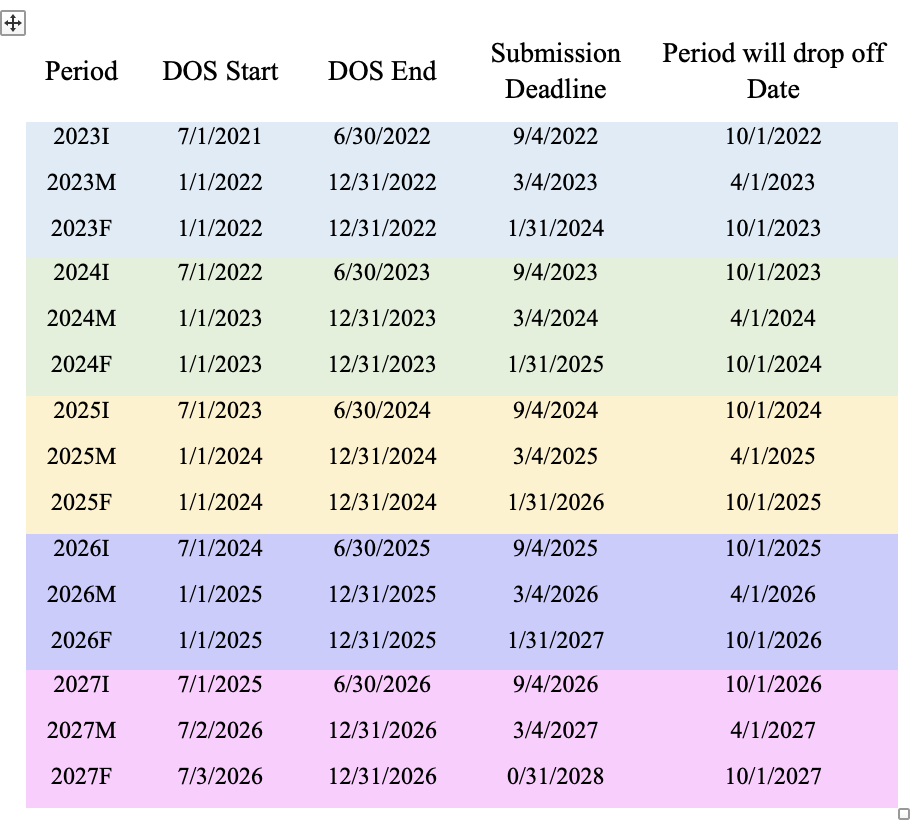
Each year, CMS “freezes” claim and encounter data three times to re-calibrate member MRA scores according to the reviews previously discussed. There are the initial, mid-year and final reconciliation periods (in the table below, these are abbreviated to I, M and F under “Period”).
For your reference, deadlines between 2023-2027 can be found in the table below.
Want a tool to help you calculate MRA scores? Try the new MRA Calculator.
The MRA Calculator is a tool created to helps coders and analysts quickly and accurately prioritize which chart they’d like to audit. The MRA Calculator adjusts the Medicare Risk Adjusted rate as you enter patient demographic information and HCC codes into the chart. Additionally, users can search by code or description and save the end report as a PDF.